How can TATO help me in ablation?
During the past 20 years, the objectives of ablation research endpoints have been to increase ablation
volumes while reducing the procedural times and increasing the reproducibility. This means higher
wattage, cooling optimization and larger calibre antennas. Large volumes of coagulative necrosis,
however, are not the only achievement that matters in daily clinical practice. While ablation can be considered a minimally invasive treatment, some risks exist and the principle
of beneficence against the principle of non-maleficence should be evaluated in order to optimize
the treatment, balancing safety and efficacy. By planning an ablation treatment, it is fundamental to
take into consideration the presence of factors affecting treatment safety or efficacy.
Liver Ablation
Treating Patients at high risk of bleeding
Among the potential complications affecting safety, bleeding is the most important to be prevented.
Unlike surgeons, Interventional Radiologists do not have direct control of haemostasis. For this reason,
ablation is considered as a high bleeding-risk procedure[1].
When abnormalities in the coagulation are present, the risk of the occurrence of perihepatic free
fluid after intervention or complications of any kind during follow-up is increased[2]. The availability of
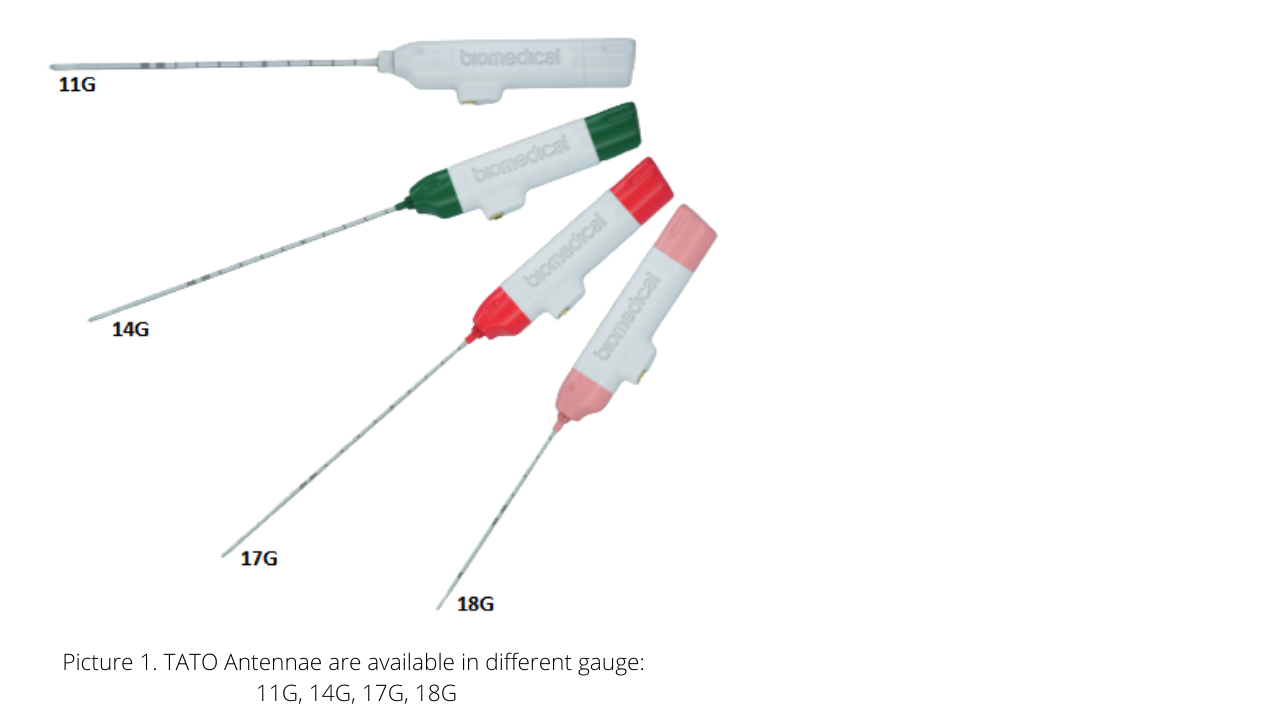
thinner antennas may be useful in patients at risk, such as those with cirrhosis, abnormal platelets, or
elevated values of INR.
Treating Nodules at high risk of bleeding and/or seeding
Nodules in subcapsular location treated with a direct
puncture are at higher risk of bleeding and seeding. The
latter especially if the nodule is not well differentiated
or presents an invasive tumoral pattern[3]. Therefore, in
the treatment of subcapsular nodules, direct puncture
should be avoided.
In the impossibility of interposing healthy parenchyma,
“no touch” technique has been demonstrated as feasible
and useful[4]. Multi-antenna microwave devices can be
useful in nodules with subcapsular location and every
time the physician prefers a no-touch technique.

Treating Nodules located near critical structures
Undesirable thermal damage can also affect safety and a “controlled ablation”, not growing too fast
and too much in length is desirable. Structures that can be damaged are represented by:
- Muscles. Pain may follow ablation for several days or weeks.
- Main biliary tree. It is possible to perform the cooling of main biliary ducts,
even if this procedure is not easy and practical[5]
- Surrounding viscera, such as the colon or the gallbladder. In such locations,
it is advisable to use artificial ascites Dextrose 5% for Radiofrequency (RF) or 0,9%
NaCl for Microwave (MW)[6] but it is not always effective. When MW ablation is performed,
significant tissue retraction can occur. The use of high power can sometimes induce
an important tissue retraction, attracting the viscera near the ablation area even
if it has not been classified as a structure at risk at the beginning of the treatment.
%20view%20under%20US%20before%20hydro%20dissection.png)
In all those situations, a “controlled ablation” is desirable. While RF ablation is a mild, more controlled,
and slowly growing technique, controlled MW ablation should be preferred due to its physical
properties. Microwave tissue heating relies on the interaction of an electromagnetic field with water
molecules in the tissue, while radiofrequency tissue heating is produced by an electric current going
through the needles and the patient[7]. RF heating is limited in areas of low electrical conductivity (where
there are no ions to be flipped), such as in the lung or in the bone. On the contrary, MW are capable of
propagating more effectively, heating tissues with low electrical conductivity, (high impedance) or low
thermal conductivity. Unlike RF, MW heating expands beyond charred or desiccated tissues[8]. MW are also
less sensitive to the phenomenon of heat sink effect, that consists in the presence of flowing blood causing
a cooling effect, thereby reducing the ablation volume[9].
Beyond the liver
Lung Ablation
Pneumothorax is the most frequent complication of ablation of primary and secondary lung tumors[10].
It has been demonstrated, in lung biopsy series, that the rate of pneumothorax is related to the calibre
of the needle used to puncture the lung[11]. Due to the ability of MW to propagate effectively and heat
tissues with low electrical conductivity, high impedance or low thermal conductivity such as the lung,
the combination of thin antennae and MW energy delivery could provide better results in lung ablation[12] (Picture 5).
This is especially true in case of small lung nodules such as metastases, which are often difficult to
puncture as they might move” in lung parenchyma when touched by the antenna (Picture 6). The antenna
can be placed on the side of the nodule and MW energy can effectively propagate and ablate the nodule
and the tissue.
Thyroid Ablation
Ablation of benign thyroid nodules or recurrencies of malignant thyroid neoplasms requires the
availability of thin and short devices, and the possibility to carefully monitor the treatment[13]. These
treatments are usually performed under ultrasound (US) guidance: devices with optimal echogenicity
and a slow-growing controlled treatment induced hyper echogenicity are mandatory for a safe
treatment. MW could overcome limitations of RF in treating highly vascularized benign or malignant
nodules, due to its physical properties[14].
- 18G x 8 cm length TATO antenna is specifically designed for thyroid ablation.
It is highly visible under US and the thermal induced hyper echogenicity
grows slowly and in a controlled way
Currently there are many ablation devices with inherent differences. It is important to know these
differences, in order to match the patient/nodule with the correct ablation technique and to balance
power and control. TATO may offer advantages in combining MW energy delivered in a controlled
fashion and less invasive approach.
References
1. Patel IJ, Rahim S, Davidson JC, et al. Society of Interventional Radiology Concensus Guidelines for the Periprocedural Management of Thrombotic and Bleeding Risk in
Patients undergoing Percutaneous Image-Guided Interventions - Part II: Recommendations. Endorsed by the Canadian Association for Interventional Radiology and the
Cardiovascular and Interventional Radiology Society of Europe. J Vasc Interv Radiol. 2019; 30:1168-1184.
2. Biondetti P, Fumarola EM, Ierardi AM, et al. Percutaneous US-guided MWA of small liver HCC: predictors of outcome and risk factors for complications from a single
center experience. Medical Oncology. 2020; 5:37-39
3. Bruix J et Llovet JM. Prognostic Prediction and Treatment Strategy in Hepatocellular Carcinoma. Hepatology. 2001; 33:1124-1129
4. Kawamura Y, Ikeda K, Fukushima T, et al. Potential of a no-touch pincer ablation procedure for small hepatocellular carcinoma that uses a multipolar radiofrequency
ablation system: An experimental animal study. Hepatol Research. 2014; 44:1234-40.
5. Elias D, Sideris L, Pocard M, et al. Intraductal cooling of the. main bile ducts during radiofrequency ablation prevents biliary stenosis. J Am. Coll Surg. 2004; 198(5):717-21.
6. Kondo Y, Yoshida H, Shiina S, et al. Artificial ascites technique for percutaneous radiofrequency ablation of liver cancer adjacent to the gastrointestinal tract. Br J
Society. 2006; 93(10):1277-1282.
7. Lubner MG, Brace CL, Hinshaw JL, et al. Microwave tumor ablation: mechanism of action, clinical results, and devices. J Vasc Interv Radiol. 2010; 21(8):192-203.
8. Brace CL. Microwave ablation technology: what every user should know. Curr Probl Diagn Radiol. 2009; 38(2):61-7.
9. Dodd III GD, Dodd NA, Lanctot AC, et al. Effect of Variation of Portal Venous Blood Flow on Radiofrequency and Microwave Ablations in a Blood-perfused Bovine Liver
Model. Radiology. 2013; 267:129-136
10. De Baere T, Auperin A, Deschamps F, et al. Radiofrequency ablation is a valid treatment option for lung metastases: experience in 566 patients with 1037 metastases.
Annals of Oncology. 2015;26: 987–991
11. Huo YR, Chan MV, Habib AR, Lui I, Ridley L. Pneumothorax rates in CT-Guided lung biopsies: a comprehensive systematic review and meta-analysis of risk factors. Br J
Radiol. 2020;93(1108):20190866
12. Iezzi R, Cioni R, Basile D, et al. Standardizing percutaneous Microwave Ablation in the treatment of Lung Tumors: a prospective multicenter trial (MALT study). Eur
Radiol. 2020 Sep 30. doi: 10.1007/s00330-020-07299-2
13. Cervelli R, Mazzeo S, De Napoli L, et al. Radiofrequency Ablation in the Treatment of Benign Thyroid Nodules: An Efficient and Safe Alternative to Surgery. J Vasc Interv
Radiol. 2017;28:1400-1408
14. Teng D, Ding L, Wang Y, Liu C, Xia Y, Wang H. Safety and efficiency of ultrasound-guided low power microwave ablation in the treatment of cervical metastatic lymph
node from papillary thyroid carcinoma: a mean of 32 months follow-up study. Endocrine. 2018 Dec;62(3):648-654.
